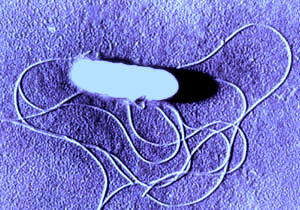
Listeria (pronounced liss-STEER-ē-uh) is a gram-positive rod-shaped bacterium that can grow under either anaerobic (without oxygen) or aerobic (with oxygen) conditions. Of the six species of Listeria, only L. monocytogenes (pronounced maw-NO-site-aw-JUH-neez) causes disease in humans. These bacteria multiply best at 86-98.6 degrees F (30-37 degrees C), but also multiply better than all other bacteria at refrigerator temperatures, something that allows temperature to be used as a means of differentiating Listeria from other contaminating bacteria.
Called an “opportunistic pathogen,” Listeria is noted to cause an estimated 2,600 cases per year of severe invasive illness. Perhaps not surprisingly then, “foodborne illness caused by Listeria monocytogenes has raised significant public health concern in the United States, Europe, and other areas of the world.” As one noted expert observed, summarizing the history of these bacteria and their significance for public health:
Although L. monocytogenes was recognized as an animal pathogen over 80 years ago, the first outbreak confirming an indirect transmission from animals to humans was reported only in 1983, in Canada’s Maritime provinces. In that outbreak, cabbages, stored in the cold over the winter, were contaminated with Listeria through exposure to infected sheep manure. A subsequent outbreak in California in 1985 confirmed the role of food in disseminating listeriosis. Since then Listeria has been implicated in many outbreaks of food-borne illness, most commonly from exposure to contaminated dairy products and prepared meat products, including turkey and deli meats, pâté, hot dogs and seafood and fish.
Given its widespread presence in the environment and food supply, the ingestion of Listeria has been described as an “exceedingly common occurrence.”
Transmission and Infection
Except for the transmission of mother to fetus, human-to-human transmission of Listeria is not known to occur. Infection is caused almost exclusively by the ingestion of the bacteria, most often through the consumption of contaminated food. The most widely-accepted estimate of foodborne transmission is 85-95% of all Listeria cases
The infective dose—that is, the amount of bacteria that must be ingested to cause illness—is not known. In an otherwise healthy person, an extremely large number of Listeria bacteria must be ingested to cause illness—estimated to be somewhere between 10–100 million viable bacteria (or colony forming units “CFU”) in healthy individuals, and only 0.1–10 million CFU in people at high risk of infection. Even with such a dose, a healthy individual will suffer only a fever, diarrhea, and related gastrointestinal symptoms.
The amount of time from infection to the onset of symptoms—typically referred to as the incubation period—can vary to a significant degree. Symptoms of Listeria infection can develop at any time from 2 to 70 days after eating contaminated food. According to one authoritative text:
The incubation period for invasive illness is not well established, but evidence from a few cases related to specific ingestions points to 11 to 70 days, with a mean of 31 days. In one report, two pregnant women whose only common exposure was attendance at a party developed Listeria bacteremia with the same uncommon enzyme type; incubation periods for illness were 19 and 23 days.
Adults can get listeriosis by eating food contaminated with Listeria, but babies can be born with listeriosis if their mothers eat contaminated food during pregnancy. The mode of transmission of Listeria to the fetus is either transplacental via the maternal blood stream or ascending from a colonized genital tract. Infections during pregnancy can cause premature delivery, miscarriage, stillbirth, or serious health problems for the newborn.
Incidence of Listeria infection in HIV-positive individuals is higher than in the general population. One study found that:
The estimated incidence of listeriosis among HIV-infected patients in metropolitan Atlanta was 52 cases per 100,000 patients per year, and among patients with AIDS it was 115 cases per 100,000 patients per year, rates 65–145 times higher than those among the general population. HIV-associated cases occurred in adults who were 29–62 years of age and in postnatal infants who were 2 and 6 months of age.
Pregnant women make up around 30% of all infection cases, while accounting for 60% of cases involving the 10- to 40-year age group.
Symptoms of Listeria infection
When a person is infected and develops symptoms of Listeria infection, the resulting illness is called listeriosis. Only a small percentage of persons who ingest Listeria fall ill or develop symptoms. For those who do develop symptoms as a result of their infection, the resulting illness is either mild or quite severe—sometimes referred to as a “bimodal distribution of severity.”
On the mild end of the spectrum, listeriosis usually consists of the sudden onset of fever, chills, severe headache, vomiting, and other influenza-type symptoms. Along these same lines, the CDC notes that infected individuals may develop fever, muscle aches, and sometimes gastrointestinal symptoms such as nausea or diarrhea. When present, the diarrhea usually lasts 1-4 days (with 42 hours being average), with 12 bowel movements per day at its worst.
Most healthy adults and children who consume contaminated food experience only mild to moderate symptoms. The infection is usually self-limited, since, in healthy hosts, exposure to Listeria stimulates the production of tumour necrosis factor and other cytokines, which activate monocytes and macrophages to eradicate the organism. Few people with normal immune function go on to have more severe, life-threatening forms of listeriosis, characterized by septic shock, meningitis and encephalitis.
As already noted, when pregnant, women have a mildly impaired immune system that makes them susceptible to Listeria infection. If infected, the illness appears as an acute fever, muscle pain, backache, and headache. Illness usually occurs in the third trimester, which is when immunity is at its lowest. Infection during pregnancy can lead to premature labor, miscarriage, infection of the newborn, or even stillbirth. Twenty-two percent of such infections result in stillbirth or neonatal death.
Newborns may present clinically with early-onset (less than 7 days) or late-onset forms of infection (7 or more days). Those with the early-onset form are often diagnosed in the first 24 hours of life with sepsis (infection in the blood). Early-onset listeriosis is most often acquired through trans-placental transmission. Late-onset neonatal listeriosis is less common than the early-onset form. Clinical symptoms may be subtle and include irritability, fever and poor feeding. The mode of acquisition of late-onset listeriosis is poorly understood.
Diagnosis and Treatment of Listeria Infections
Because there are few symptoms that are unique to listeriosis, doctors must consider a variety of potential causes for infection, including viral infections (like flu), and other bacterial infections that may cause sepsis or meningitis.
Early diagnosis and treatment of listeriosis in high-risk patients is critical, since the outcome of untreated infection can be devastating. This is especially true for pregnant women because of the increased risk of spontaneous abortion and preterm delivery. Depending on the risk group, rates of death from listeriosis range from 10% to 50%, with the highest rate among newborns in the first week of life.
Methods typically used to identify diarrhea-causing bacteria in stool cultures interfere or limit the growth of Listeria, making it less likely to be identified and isolated for further testing. On the other hand, routine methods are effective for isolating Listeria from spinal fluid, blood, and joint fluid. Magnetic-resonance imaging (MRI) is used to confirm or rule out brain or brain stem involvement.
Listeriosis is usually a self-limited illness—which means that a majority of infected individuals will improve without the need for medical care. But for those patients with a high fever, a stool culture and antibiotic-treatment may be justified for otherwise healthy individuals. Although there have been no studies done to determine what drugs or treatment duration is best, ampicillin is generally considered the “preferred agent.” There is no consensus on the best approach for patients who are allergic to penicillins.
Invasive infections with Listeria can be treated with antibiotics. When infection occurs during pregnancy, antibiotics given promptly to the pregnant woman can often prevent infection of the fetus or newborn. Babies with listeriosis receive the same antibiotics as adults, although a combination of antibiotics is often used until physicians are certain of the diagnosis.
Those Most Susceptible to Infection
Several segments of the population are at increased risk and need to be informed so that proper precautions can be taken. The body’s defense against Listeria is called “cell-mediated immunity” because the success of defending against infection depends on our cells (as opposed to our antibodies), especially lymphocytes called “T-cells.” Therefore, individuals whose cell-mediated immunity is suppressed are more susceptible to the devastating effects of listeriosis, including especially HIV-infected individuals, who have been found to have a Listeria-related mortality of 29%.
Pregnant women naturally have a depressed cell-mediated immune system. In addition, the immune systems of fetuses and newborns are very immature and are extremely susceptible to these types of infections. Other adults, especially transplant recipients and lymphoma patients, are given necessary therapies with the specific intent of depressing T-cells, and these individuals become especially susceptible to Listeria as well.
According to the CDC and other public health organizations, individuals at increased risk for being infected and becoming seriously ill with Listeria include the following groups:
- Pregnant women: They are about 20 times more likely than other healthy adults to get listeriosis. About one-third of listeriosis cases happen during pregnancy.
- Newborns: Newborns rather than the pregnant women themselves suffer the serious effects of infection in pregnancy.
- Persons with weakened immune systems
- Persons with cancer, diabetes, or kidney disease
- Persons with AIDS: They are almost 300 times more likely to get listeriosis than people with normal immune systems.
- Persons who take glucocorticosteroid medications (such as cortisone)
- The elderly
Complications of Listeria infection
For those persons who suffer a Listeria infection that does not resolve on its own, the complications (or sequelae) can be many. The most common is septicemia (bacterial pathogens in the blood, also known as bacteremia), with meningitis being the second most common. Other complications can include inflammation of the brain or brain stem (encephalitis), brain abscess, inflammation of the heart-membrane (endocarditis), and localized infection, either internally or of the skin.
Death is the most severe consequence of listeriosis, and it is tragically common. For example, based on 2009 FoodNet surveillance data, 89.2% of Listeria patients ended up in the hospital, the highest hospitalization rate for pathogenic bacterial infection. In persons 50 years of age and older, there was a 17.5% fatality rate—also the highest relative to other pathogens.
The Incidence of Listeria Infections
Listeria bacteria are found widely in the environment in soil, including in decaying vegetation and water, and may be part of the fecal flora of a large number of mammals, including healthy human adults. According to the FDA, “studies suggest that 1-10% of humans may be intestinal carriers of Listeria.” Another authority notes that the “organism has been isolated from the stool of approximately 5% of healthy adults.” Overall, seasonal trends show a notable peak in total Listeria cases and related-deaths from July through October.
Ingested by mouth, Listeria is among the most virulent foodborne pathogens, with up to 20% of clinical infections resulting in death. These bacteria primarily cause severe illness and death in persons with immature or compromised immune systems. Consequently, most healthy adults can be exposed to Listeria with little to any risk of infection and illness.
A study published in 1995 projected Listeria infection-rates to the U.S. population, suggesting that an estimated 1,965 cases and 481 deaths occurred in 1989 compared with an estimated 1,092 cases and 248 deaths in 1993, a 44% and 48% reduction in illness and death, respectively. In comparison, a USDA study published in 1996 estimated that there had been 1,795-1860 Listeria-related cases in 1993, and 445-510 deaths, with 85-95% of these attributable to the consumption of contaminated food. Listeriosis-related mortality rates decreased annually by 10.7% from 1990 through 1996, and by 4.3% from 1996 through 2005.
Among adults 50 years of age and older, infection rates were estimated to have declined from 16.2 per 1 million in 1989 to 10.2 per 1 million in 1993. Perinatal disease decreased from 17.4 cases per 100,000 births in 1989 to 8.6 cases per 100,000 births in 1993. Neonatal infections are often severe, with a mortality rate of 25-50%.
According to the CDC’s National Center for Zoonotic, Vector-Borne, and Enteric Diseases:
Listeriosis was added to the list of nationally notifiable diseases in 2001. To improve surveillance, the Council of State and Territorial Epidemiologists has recommended that all L. monocytogenes isolates be forwarded to state public health laboratories for subtyping through the National Molecular Subtyping Network for Foodborne Disease Surveillance (PulseNet). All states have regulations requiring health care providers to report cases of listeriosis and public health officials try to interview all persons with listeriosis promptly using a standard questionnaire about high risk foods. In addition, FoodNet conducts active laboratory- and population-based surveillance.
In 2006, public health officials from 48 states reported 1,270 foodborne disease outbreaks, with a confirmed or suspect source in 884 of the outbreaks (70%). Only one of the outbreaks with a confirmed source was attributed to Listeria, with this outbreak involving eleven hospitalizations and one death. The next year, of 17,883 lab-confirmed infections, the CDC attributed 122 to Listeria. In 2009, there were 158 confirmed Listeria infections, representing an incidence-rate of .34 cases for every 100,000 persons in the United States. Such data revealed an incidence-rate of 0.27 cases per 100,000 persons, a decrease of 42% compared with 1996—1998. But, according to CDC’s Technical Information website, it is estimated that there are 1,600 cases of Listeria infection annually in the United States, based on data through 2008.
The 2009 numbers represented a reported 30% decrease in the number of infections compared to the 1996—1998 rates of infection. Although the nature and degree of underreporting is subject to dispute, all agree that the confirmed cases represent just the tip of the iceberg. Indeed, one study estimates the annual incidence rate for Listeria to be around 1,795-1,860 cases per 100,000 persons, with 445-510 of the cases ending in death.
Finally, in a study of FoodNet laboratory-confirmed invasive cases—where infection is detected in blood, cerebrospinal fluid, amniotic fluid, placenta or products of conception—the number of listeriosis cases decreased by 24% from 1996 through 2003. During this same period, pregnancy-associated disease decreased by 37%, while cases among those fifty years old and older decreased by 23%.
Marler Clark, The Food Safety Law Firm, is the nation’s leading law firm representing victims of Listeria outbreaks. The Listeria lawyers of Marler Clark have represented thousands of victims of Listeria and other foodborne illness outbreaks and have recovered over $600 million for clients. Marler Clark is the only law firm in the nation with a practice focused exclusively on foodborne illness litigation. Our Listeria lawyers have litigated Listeria cases stemming from outbreaks traced to a variety of foods, such as caramel apples, cantaloupe, cheese, celery and milk.